Nursing Care Plan for Gastroesophageal Reflux Disease (GERD)
Introduction:
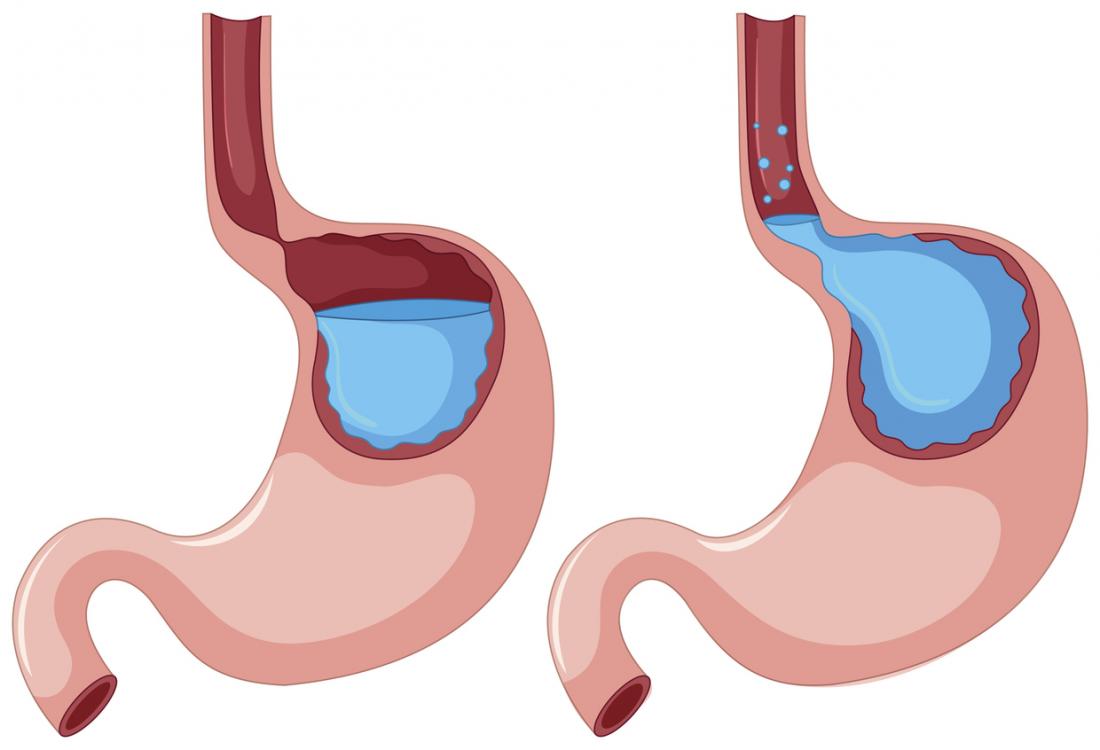
Gastroesophageal reflux disease (GERD) is a chronic condition characterized by the backflow of stomach acid and contents into the esophagus. It can cause discomfort, pain, and other symptoms. As a nurse, your role is vital in managing GERD symptoms, providing education, and promoting lifestyle modifications. This nursing care plan aims to outline evidence-based interventions to assess, manage, and support patients with GERD.
Patient Assessment:
- Name: [Patient’s Name]
- Age: [Patient’s Age]
- Gender: [Patient’s Gender]
- Medical History: [Brief summary of patient’s medical history]
- The severity of GERD: [Mild, moderate, or severe]
- Medical Diagnosis: Gastroesophageal Reflux Disease (GERD)
- Date of Admission: [Date of Admission]
- Date of Care Plan: [Date of Care Plan]
GERD Nursing Diagnosis:
- Acute Pain related to esophageal irritation and inflammation.
- Imbalanced Nutrition: Less than Body Requirements related to decreased appetite, avoidance of certain foods, and potential weight loss.
- Deficient Knowledge regarding GERD triggers, and self-care measures.
- Risk for Aspiration related to reflux of gastric contents into the respiratory system.
- Acute Pain related to gastric acid reflux and esophageal irritation as evidenced by the patient’s verbalization of heartburn or chest pain.
- Impaired Swallowing related to esophageal inflammation and discomfort as evidenced by the patient’s report of difficulty swallowing or feeling of food getting stuck.
- Deficient Knowledge related to the management of GERD and lifestyle modifications as evidenced by the patient’s request for information and lack of understanding about triggers and self-care strategies.
GERD Nursing Interventions:
Acute Pain:
- Assess the patient’s pain level, location, and characteristics regularly.
- Administer prescribed medications, such as antacids, proton pump inhibitors, or H2 receptor antagonists, to reduce gastric acidity and alleviate pain.
- Encourage the patient to adopt an upright position or elevate the head of the bed to reduce reflux and minimize pain.
- Provide education on relaxation techniques, stress reduction, and lifestyle modifications to manage pain effectively.
- Assess the patient’s pain level using a pain scale and ask about the location, intensity, and quality of the pain.
- Administer prescribed antacids, proton pump inhibitors, or H2 receptor antagonists as ordered to provide relief from heartburn and reduce gastric acid production.
- Encourage the patient to avoid trigger foods and beverages that may worsen symptoms, such as spicy foods, caffeine, and alcohol.
- Assist the patient in finding a comfortable position, such as elevating the head of the bed, to minimize acid reflux during sleep.
- Collaborate with the healthcare team to explore additional pain management strategies, such as relaxation techniques or non-pharmacological interventions.
Imbalanced Nutrition: Less than Body Requirements:
- Assess the patient’s nutritional status, dietary habits, and weight changes.
- Collaborate with the healthcare team, including a registered dietitian, to develop an individualized nutrition plan that addresses the patient’s specific needs.
- Educate the patient about trigger foods to avoid, such as fatty or spicy foods, caffeine, chocolate, and citrus fruits.
- Encourage the patient to consume smaller, frequent meals and avoid lying down immediately after eating to minimize reflux symptoms.
Impaired Swallowing:
- Assess the patient’s ability to swallow and any associated difficulties.
- Collaborate with a speech-language pathologist to assess swallowing function and provide appropriate interventions, such as swallowing exercises or dietary modifications.
- Encourage the patient to eat smaller, more frequent meals and chew food thoroughly to facilitate swallowing and reduce the risk of reflux.
- Educate the patient about maintaining an upright posture while eating and avoiding lying down immediately after meals to prevent acid reflux.
- Provide nutritional counseling to ensure the patient is consuming a balanced diet that is low in fat and acidic foods.
Deficient Knowledge:
- Assess the patient’s understanding of GERD, including its causes, triggers, and potential complications.
- Provide education on GERD, emphasizing the importance of lifestyle modifications, such as weight management, smoking cessation, and avoiding trigger foods and beverages.
- Teach the patient about medications prescribed for GERD and the importance of adhering to the prescribed regimen.
- Offer written materials, reliable resources, or referrals to support groups for additional information and ongoing support.
Risk for Aspiration:
- Assess the patient’s respiratory status, including lung sounds, oxygen saturation, and signs of respiratory distress.
- Position the patient in an upright position during and after meals to reduce the risk of aspiration.
- Encourage the patient to eat slowly, chew food thoroughly, and take small bites to prevent choking and aspiration.
- Monitor for signs of respiratory complications, such as coughing, wheezing, or shortness of breath, and promptly report to the healthcare team.
GERD Nursing Evaluation:
- Relief of acute pain associated with GERD.
- Achievement of balanced nutrition and prevention of malnutrition-related complications.
- Increased knowledge and understanding of GERD triggers, lifestyle modifications, and self-care measures.
- Prevention of aspiration-related complications through positioning and education.
- The patient experiences a reduction in heartburn and chest pain.
- The patient demonstrates improved swallowing function and reports less difficulty with swallowing.
- The patient expresses an understanding of GERD triggers and management strategies, including lifestyle modifications.
- The patient actively engages in self-management strategies and seeks appropriate support when needed.
Documentation:
Regularly document the patient’s pain assessments, nutritional status, educational interventions, and the patient’s response to treatment. Collaborate with the interdisciplinary healthcare team to review and update the care plan based on the patient’s condition and evolving needs.
Note: This nursing care plan is a general guideline and should be individualized based on the patient’s specific needs, the severity of GERD, the treatment plan, and the healthcare provider’s recommendations.

One Response
Your diagnosis is useful for me thanku so much 🥰